last authored: Oct 2016, Samantha Allison, David LaPierre
Introduction
Choking occurs when a foreign object becomes lodged in the throat or trachea (windpipe), causing an obstruction and blocking the flow of air. There are two types of choking; partial airway obstruction and total airway obstruction.
People of all ages can have difficulties with chewing and swallowing, but children and the elderly are at highest risk. These risk factors occur due to normal aging processes; effects of medications; dental issues; and health conditions such as dementia, Parkinson’s disease, and multiple sclerosis (HealthLinkBC, 2015).
Causes and Risk Factors
Airway obstruction most frequently occurs when food or another object becomes lodged in the airway. It may also be caused by blood or vomit, as well as the tongue if the patient has decreased level of consciousness.
Risk Factors include:
- Difficulty swallowing or chewing
- People with neurological illnesses; diseases that cause muscular degeneration, such as MS; disorders of the esophagus such as a narrowed esophagus due to chronic acid reflux (GERD)
- Eating too quickly, eating while distracted, and/or not chewing food properly
- Eating while in supine position
- Poor positioning
- Medication side effects – dry mouth, relaxed muscle tone, increased salivation
- Alcohol and sedating drugs
- Poor oral hygiene
- Ill-fitting dentures
- Incorrect food texture/fluid consistency for the person’s ability
Assessment of Choking
The universal sign for choking is hand(s) around or clutched to the throat. Signs and symptoms of choking include:
- struggling to breathe
- gasping
- coughing or gagging
- bluish lips or skin
- anxiety or agitation
Airway obstruction should be considered if the patient becomes suddenly and extremely unwell, or if they are found unresponsive.
Other indications of choking can be used to determine whether there is a partial or total airway obstruction.
| Partial Airway Obstruction | Total Airway Obstruction |
| Responsive and can cough forcefully | Inability to speak or breathe |
| Laboured air exchange – respirations gasping or noisy | Poor or no air exchange; high-pitched noise while inhaling or no noise at all |
| May wheeze between coughs | Weak, ineffective cough or no cough at all |
| Reddened face; pale or blueish skin colour if prolonged | Cyanosis of skin, lips, fingernails and earlobes |
Management
Recognize the problem – Approach the patient and identify yourself. Assess for airway obstruction and call out for assistance if needed.
Offer your assistance – Ask the patient “Are you choking?” and “can I help?” This will help determine if the airway if completely obstructed.
Partial Obstruction
If the person can cough, speak, or breathe and you suspect a partial obstruction, do not interfere. Never use back blows on someone that can cough or breathe.
Total Obstruction – Responsive
5 back blows – If a complete obstruction is suspected and the person is responsive, deliver 5 blows on the patient’s back with the heel of your hand. Your hand should make contact right between the shoulder blades.
Landmark the Abdomen – If back blows are ineffective, stand behind the choking patient and wrap your arms around the waist. Place the thumb side of your fist on their abdomen, midline above navel, ensuring you are positioned well below breast bone.
5 abdominal thrusts – Grab your fist with your other hand and deliver 5 quick, forceful upward thrusts. Continue alternating between 5 back blows and 5 abdominal thrusts until the patient begins coughing, the object becomes dislodged, or patient becomes unresponsive.
Special consideration: For an obese or pregnant person, perform a combination of 5 back blows and 5 chest thrusts.
Total Obstruction – Unresponsive
An unresponsive patient should be managed supine. Assist patient to the floor, ensuring you are protecting the head and neck as you do so.
Initiate CPR – Place two hands on the patient’s chest and administer 30 chest compressions.
Head tilt/chin lift – Assess the mouth. If a foreign object is visible, carefully remove it by using the finger-sweep technique. Stop immediately if it appears that the object is being pushed deeper into the airway.
Rescue breathing – Give two breaths to the patient. If the first breath does not go in, reposition the airway by repeating head tilt/chin lift maneuver. Assess the mouth again for an object and if nothing visible, attempt a second breath.
Continue CPR – Continue providing CPR if airway remains blocked or if patient is still not breathing. The object may dislodge during chest compressions, so ensure that you are rechecking the mouth.
If the obstruction is dislodged and patient is breathing, provide on-going care.
Closely monitor level of consciousness and breathing. Place the patient on their side into the recovery position, and treat for symptoms of shock.
Stay with the patient until emergency medical services arrive.
Advanced Management
Children and Infants
A child of sufficient age should be managed according to adult procedures. If the child is too small to stand, alternating back blows and chest compressions may be used.
Laryngoscopy
If you have the qualifications and equipment, laryngoscopy may be attempted in order to visualize and remove an obstruction. A laryngoscope should be inserted according to the procedure described under Advanced Airway Management.
Next, the obstruction may be removed, using suction or Macgill forceps.
Cricothyroidotomy
A final attempt at securing an airway under emergency circumstances may be made surgically, using needle or open cricothyroidotomy. Both procedures use the cricoid cartilage, which is located below the prominence of the thyroid cartilage.
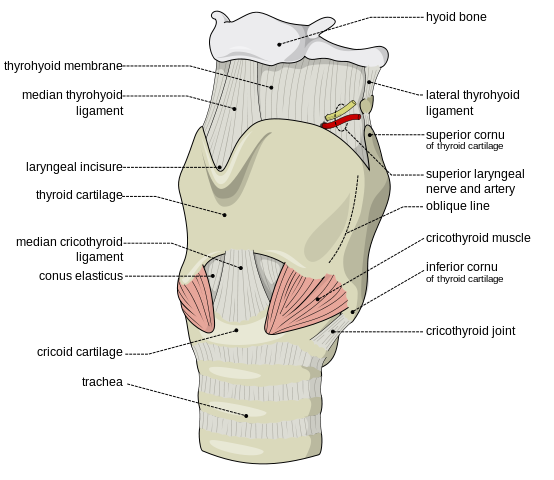
courtesy of Olek Remesz
Needle cricothyroidotomy involves inserting a large bore (12-14G) needle at an oblique angle through the cricoid membrane. This may provide temporary opportunity for jet oxygenation, but needs to be followed by more definitive securing of the airway within 30-60 min.
Open cricothyroidotomy involves a vertical incision through the skin over the cricoid membrane, followed by dissection down to the membrane. A horizontal cut is then made through the cricoid membrane, with a retractor or the scalpel handle used to maintain the airway before an endotracheal tube is inserted.

courtesy of Svenriviere
A cricothyroidotomy kit, using the Seldinger technique may be available in some settings.
Prevention
The risk of choking can be reduced with certain interventions. Health care providers should:
- ensure that the patient is receiving the proper food texture and fluid consistency
- ensure the patient is positioned properly and has the appropriate adaptive eating devices if required
- ensure the patient is awake and alert and avoids talking when chewing or swallowing
- encourage or provide patient with good oral hygiene. Ensure dentures are in place and well fitted.
- refer to a registered dietician or a speech language pathologist if patient is having difficulty with swallowing or chewing
Resources and References
HealthLinkBC. (2015). Managing chewing and swallowing difficulties in care facilities.
PERRI-MED FIRST AID AND CPR TRAINING. (2011). CPR. In Basic life support for lay rescuers (7th ed., pp. 1-57). : Perri-Med First Aid/CPR Training.
