last authored: Aug 2016, Andrew Bridgen, Karly Kreitzer
Introduction
Clinical references provided below
This article discusses the role of potent medications called vasopressors and inotropes, used to support cardiovascular function during resuscitation and other critical times. These medications activate adrenergic and dopaminergic receptors in the heart and vasculature to affect a number of critical physiologic parameters:
- Vasoconstriction of vascular smooth muscle, thereby increasing blood pressure
- Inotropy: increasing contractility of cardiomyocytes
- Chronotropy: increasing the heart rate (via SA node)
- Dromotropy: increasing the conduction velocity within the heart (via AV node)
Medications are described according to their primary effect:
- Vasopressors increase vasoconstriction
- Inotropes increase cardiac contractility
- Inodilators increase cardiac contractility, while also causing vasodilation
These drugs are incredibly potent, and should only be used in a monitored setting with expert oversight. Nevertheless, they can also be life-saving, and all health care providers who may be involved in resuscitation should have a degree of familiarity with these medications.
Adrenergic and Dopamine Receptor Physiology
Main articles: heart as a pump, blood pressure
courtesy of Sven Jahnichen
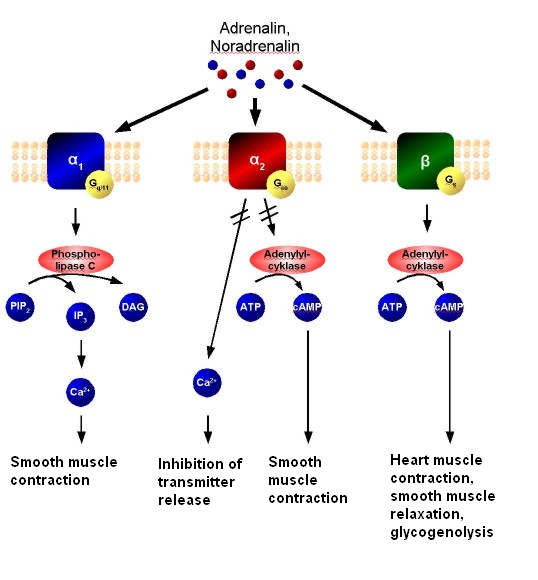
Adrenergic receptors exist on the cell membranes in a wide variety of tissues and mediate response to the sympathetic nervous system – principally the catecholamines epinephrine and norepinephrine. There are at least five receptor types, located in various tissues and with different physiologic effects. These receptors are G-protein coupled receptors; their activation results in rapid signal transduction through the cell, as described in the image.
Activation of adrenergic receptors may have a number of physiological impacts within the cardiovascular system, including:
- Vasoconstriction of vascular smooth muscle, thereby increasing blood pressure
- Inotropy: increasing contractility of cardiomyocytes
- Chronotropy: increasing the heart rate (via SA node)
- Dromotropy: increasing the conduction velocity within the heart (via AV node)
Effects of specific receptor types are described in the table below.
Dopamine is another neurotransmitter that has cardiovascular effects. It increases vasodilation, as well as cardiac contractility through activation of at least five receptor types.
| Receptor | Tissue | Effects | Medications |
| α-1 | vascular smooth muscle | ↑ vasoconstriction | Epi, NE, Dop, PE |
| heart | ↑ inotropy | ||
| other | Prostate contraction Pupil dilation Pilomotor erection |
||
| α-2 | CNS adrenoreceptors | ↓ sympathetic outflow | Epi, NE |
| platelets | aggregation | ||
| β-1 | heart | ↑ inotropy ↑ chronotropy ↑ dromotropy |
Epi, NE, Dop, PE,Iso |
| kidney | renin release | ||
| β-2 | vascular smooth muscle | vasodilation | Epi, Dop, Iso |
| heart | ↑ inotropy ↑ chronotropy ↑ dromotropy |
Epi, NE | |
| other | Muscle: ↑ K uptake & tremors Liver glycogenolysis |
||
| β-3 | fat | lipolysis | NE, Iso |
| dopamine | vasculature | vasodilation | Dop |
Indications
While vasopressors and inotropes have a wide range of clinical uses, they are most potently used during life-threatening resuscitation, where cardiovascular collapse is threatened or has occurred.
Clinical circumstances that prompt the use of these medications include:
Cardiac
|
Non Cardiac
|
| Drug | BP | Inotropy | HR | Receptors | Indications |
| epinephrine | ↑↑ | ↑↑↑ | ↑↑↑ | α1 +++ α2 ++
β1 +++ β2 ++ |
Anaphylaxis Cardiac arrest Severe hypotension Bradycardia |
| dopamine (low dose) |
↑ | ↑ | β1 + D ++ |
||
| dopamine (med dose) |
↑ | ↑↑ | ↑↑ | α1 + β1 ++ D ++ |
|
| dopamine (high dose) |
↑↑ | ↑↑ | ↑↑ | α1 ++ β1 ++ D ++ |
|
| dobutamine | ↓ | ↑↑↑ | ↑ | α1 + β1 +++ β2 ++ |
Cardiogenic shock Severe heart failure Septic shock |
| isoproterinol | ↓ | ↑↑ | ↑↑↑ | β1 +++ β2 +++ β3 + | |
| norepinephrine | ↑↑↑ | ↑ | 0/↓ | α1 +++ α2+
β1 ++ β3 + |
Severe hypotension, especially with sepsis |
| phenylephrine | ↑↑↑ | ↑ | 0/↓ | α1 +++ | Severe hypotension |
Dosages for these medications are provided by the American Heart Association.
Practical Selection and Use
No inotropic agents have been shown to have superiority over any others in good quality trials. Use is based on cost, availability, interpretation of physiology and personal/ institutional preference.
Early Goal Directed therapy (EGDT) involves adjustments of cardiac preload, afterload, and contractility to balance oxygen delivery with oxygen demand.
Volume resuscitation should be provided aggressively when appropriate, as a circulating system without sufficient fluid will not appropriately respond to vasopressor support.
Tachyphylaxis may occur with vasopressors and inotropes. This phenomenon refers to a rapid decrease in response to medication. This desensitization leads to the need for increased doses of a drug to obtain the same effect.
Hemodynamic interactions
SC delivery in critically ill patients
Cautions, Complications, and Contraindications
Cautions
These medications are incredibly potent and can cause significant harm. They should be carefully selected, based on the clinical background, etiology, and hemodynamic parameters. They should also be slowly titrated to obtain the lowest necessary dose. Response should be frequently evaluated to allow for the shortest time interval required.
As described below, extravasation of some of these medications can cause extensive tissue damage. As such, a central line should be used when feasible; if not, a well-placed, large bore peripheral line may suffice.
Contraindications
There are no absolute contraindications for the use of vasopressors/inotropes in life-threatening conditions. Relative contraindications include preexisting cardiac arrhythmias, uncorrected hypovolemia, severe hypoxia/hypercapnia, arrhythmia secondary to cardiac glycoside intoxication, severe atherosclerosis/angina, and acute MI.
Complications
Hypoperfusion
Inadequate perfusion to the body’s extremities and vital organs can result from the excessive peripheral and visceral vasoconstriction in response to hypotension and/or vasopressors. This hypoperfusion can lead to possible tissue hypoxia, lactic acidosis and ischemic injury- with untreated hypovolemic patients being the most susceptible. In addition to excessive vasoconstriction, adrenergic agents can also increase the myocardial oxygen consumption via chronotropic and inotropic effects. Despite vasodilation effects at the heart, coronary hypoperfusion and myocardial ischemia may occur due to this increased demand in oxygen.
Arrhythmias
Vasopressors and inotropes can directly cause supraventricular tachycardias via strong chronotropic effects from stimulating adrenergic receptors, especially β-1. These agents may also indirectly cause reflex bradycardia in response to increased blood pressure. Patients with severe hypoxia/hypercapnia or concomitantly using medications that increase cardiac sensitivity are especially susceptible to these arrhythmias (See Drug Interactions).
Volume correction before vasopressor administration may limit arrhythmic frequency and severity.
Hyperglycaemia
Increased blood sugar can result from b2-adrenergic stimulation of liver cells to break down glycogen, b3-adrenergic stimulation of fat cells to break down triglycerides and possible adrenergic effects on insulin secretion/sensitivity and/or glucose uptake.
Extravasation
Extravasation into surrounding connective tissue can cause excessive local vasoconstriction with possible skin necrosis or sloughing at the injection site. Because of this, vasopressors should be administered via central vein when possible; infusions via deep antecubital vein catheters can also minimize tissue damage.
Allergies
Some formulations of adrenergic agents contain sulfites which can induce an allergic reaction (eg- anaphylaxis) in those susceptible.
Common Drug Interactions
| Drug | Applies to | Effect |
| α- and β- blocking agents | all | May ↓ effects of both agents; monitor therapy |
| Anesthetics, general
eg Halogenated HC/ Cyclopropane
|
all | May ↑ arrhythmias; if concomitant use is required, consider phenylephrine, with minimal cardiac effects |
| Antidiabetics | NE, E, DP | May ↑ hyperglycemia; monitor therapy and increase antidiabetic drug as needed |
| Atropine
|
NE, PE | May ↑ effects of norepinephrine; monitor therapy |
| Diuretics eg spironolactone |
all | May ↓ vascular response; monitor therapy |
| Digoxin | all | May ↑ arrhythmias; use extreme caution with high digoxin dosages; consider phenylephrine, with it’s decreased cardiac effects |
| MAOis | all, esp PE | May ↑ effects of α-1 agonists for up to two weeks; avoid phenylephrine, start at low doses, and closely monitor BP |
| Phenytoin (IV) | DP | May cause profound hypotension/bradycardia; consider alternative anticonvulsant and closely monitor therapy |
| Sodium nitroprusside | DB | May ↑ CO & pulmonary wedge pressure effects; monitor therapy |
Resources and References
University of Illinois ICU Guidebook
LifeInTheFastLane – Inotropes and Vasopressors
American Heart Association – Post-resuscitation Care (click on vasopressors tab)
