DRAFT – AWAITING FINAL AUTHORING
last authored: May 2016, Rushi Parikh
Introduction
A wide complex tachycardia is defined as a heart rate over 100 bpm, having a QRS complex >120msec. Pathological tachycardias may result directly from abnormal heart function, mediated by aberrant electrical activity in the atria, ventricles, or the electrical conducting system. Arrhythmias may spontaneously resolve, though they may also lead to increasingly chaotic rhythm of the heart and result in pulseless ventricular tachycardia and/or ventricular fibrillation. These signify cardiac arrest, and death will rapidly follow if defibrillation and other treatments are not provided.
Activating current originating from above ventricles that follows the electrical conduction system tends to activate the ventricles at the same time. Any aberrancy in the flow of the current that results in non-unified activation of the ventricles results in a wide complex.
Pathophysiology – General Concepts
main article: electrical control of the heart
There are many underlying processes that can lead to tachycardias.

courtesy of Angelito7
Ectopic Rhythms
If an area of tissue develops an intrinsic rate of firing faster than that of the SA node, ectopic (premature) beats can occur. They can occur due to high catecholamine concentrations, hypoxemia, ischemia, electrolyte disturbances, and drugs such as digitalis.
Abnormal Automaticity
Injured cardiomyocytes can acquire automaticity and spontaneously depolarize, though means not fully understood, but likely involving a slow calcium current.
Triggered Activity
Under certain conditions, action potentials can trigger abnormal depolarizations that result in extra heartbeats or rapid arrhythmias. Afterdepolarizations appear as oscillations and can be early, during repolarization, or delayed. Early afterdepolarizations are most common during conditions that prolong APs, such as long QT syndrome.
Reentry
Reentry occurs when impulses circulate around a unidirectional conduction block, recurrently depolarizing a region of cardiac tissue. Reentry around distinct anatomic pathways usually appears as monomorphic tachycardia on an ECG, while fibrillation is likely caused by multiple circulation reentry wave fronts.
courtesy of Life in the Fast Lane
There are many possible causes of wide complex tachycardias:
- Ventricular tachycardia: pacemaker rhythm originates within the ventricles
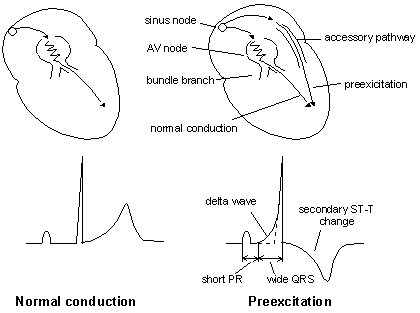
- SVT with aberrancy:
- Bundle branch blocks
- Wolf-Parkinson-White syndrome, with atrial fibrillation and an accessory pathway
Assessment
A tachycardia may represent a rapidly, life-threatening condition. Immediately assess the patient’s stability, including:
- Decreased level of consciousness
- Hypotension
- Chest pain
Do not spend undue time assessing the patient without ensuring the patient’s ABC’s (airway, breathing, and circulation) are being managed, as described under ‘basic life support‘.
History
As the patient’s stability is being ensured, ask the patient with undiagnosed tachycardia, with the following questions:
- when did it begin?
- has this ever happened before? (get details)
- is there chest pain or shortness of breath?
- have there been any syncope or presyncope?
- is there fever, chills, or other evidence of infection?
A review of systems is also warranted.
Past medical history should particularly include:
- heart disease
- thyroid disease
Social history should include:
- sleep patterns
- alcohol use
- drug use
- cigarette smoking
- caffeine intake
- stress levels
Physical Exam
Examine the patient’s overall state, including:
- level of consciousness
- vital signs
- colour
Specific attention should be paid to:
- cardiac exam
- respiratory exam
Lab Investigations
Blood work may include:
- CBC
- electrolytes
- creatinine
- troponin
- TSH
- calcium, magnesium
Diagnostic Imaging
ECG is the mainstay of imaging.
Other tests to investigate a tachycardia if the situation is non-urgent can include:
- chest X-ray (investigate for heart failure)
- echocardiogram
- holter monitor
Management – General Concepts
Treatment of tachyarrhythmias is meant to stabilize the patient, protect against lethal consequences, and mitigate the underlying cause(s) of the arrhythmia.
Call for immediate help, from experts as available.
If the patient is unstable, it is prudent to proceed immediately with synchronized cardioversion. If there is no pulse, defibrillation should be used instead. Assess and address the ABC’s when managing a patient with tachycardia. This can include:
- Opening the airway
- Providing supplemental oxygen, positive pressure ventilation, and/or intubation
- IV access x2 and fluid administration
- Chest compressions
- Defibrillation
If the patient is stable, further information may be obtained from the history, physical exam, and investigations.
Some clinicians use adenosine as a diagnostic and therapeutic tool, but it wise to consult a specialist for further management. If the rhythm is Afib and WPW, AV blocking agents may result in death.
Antiarrhythmics must be used with caution due to the high risk of further arrhythmic complications and death.
Ventricular Tachycardia with Pulse
Ventricular tachycardia (VT) is a run of three or more PVCs. Sustained VT lasts longer than 30 seconds, can induce syncope, and often requires termination by drugs or cardioversion.
Causes
Ventricular tachycardia is commonly seen in patients with structural heart disease, including myocardial infarction, heart failure, hypertrophy, electrical diseases, valvular heart diseases, and congenital heart diseases. Reentry circuits are most commonly old scars.
ECG findings
QRS complexes are wide, and occur at rates of 100-200, or sometimes faster. These wide QRS complexes distinguish ventricular tachycardia from supraventricular causes.

Courtesy of GlenLarson
Management
Idiopathic VT exists and is rarely life-threatening. However, new-onset VT is an emergency, as it can quickly deteriorate into ventricular fibrillation.
Electrical cardioversion is normally provided, especially if the patient is becoming unstable.
An alternative is medical cardioversion, including:
- Amiodarone
- Procainamide
- lidocaine
Underlying risk factors should be identified and addressed, and pacemakers are very useful for future episodes.
Torsades de Pointes
Torsades de pointes is a form of ventricular tachycardia with varying amplitudes of QRS waves.
It is usually symptomatic and can result in death, but is frequently self-limiting.
Causes
Torsades is normally associated with electrolyte imbalances, including hypokalemia or hypomagnesemia, accompanying a prolonged QT interval. This is often related to medications.
ECG Findings
The ECG image is characterized as a polymorphic wide complex tachycardia because of the asymmetry in the QRS complexes. It has also been described as “twisting on the axis” or “waxing and waning.”

Torsades, terminated by cardioversion (public domain)
Management
The mainstay of treatment is discontinuing the pre-existing medications which have caused prolonged QT intervals.
Acute treatment of this arrhythmia includes loading the patient with intravenous magnesium sulfate in addition to anti-arrhythmics, like isoproterenol and lidocaine.
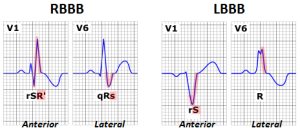
Bundle Branch Blocks
Bundle branch blocks (BBB) are defects in the conduction system within either the left or right bundle branches, leading to the characteristic wide-complex QRS complex seen on ECG. If a co-existing tachycardia occurs in a patient with a BBB, it results in a wide-complex tachycardia.
courtesy of Npatchett
After impulses travel through the AV node, they enter the bundle of His which further divides into the Right and Left bundles. The right bundle contains one fascicle, whereas the left contains two (anterior & posterior). Classification becomes more complex if specific left bundle fascicles are independently blocked. These are termed hemi-fascicular blocks, bifascicular blocks, or trifascicular blocks depending on the locations of the conduction defect.
Causes
There are several causes of BBB’s:
RBBB
|
LBBB
|
ECG Findings
The ECG findings of a BBB show a widened lateral portion on the QRS complex. With a RBBB, typically one will see the characteristic rSR’ (R ‘prime’) in lead V1 with a qRs (dominant R) in lead V6. The LBBB typically has a rS (dominant S) complex in lead V1 and the dominant RR’ in lead V6. The acronym “WiLLiaM MaRRoW” has been used to simplify this approach. William, with two “L’s” represents the LBBB. The “W” and “M” crudely represent the QRS appearance of leads 1 & 6. Marrow, therefore represents the RBBB and alternative QRS appearance.Sgarbossa criteria
Help identify new MI in a Left Bundle Branch Block
Management
Treatment of BBB’s is highly variable and completely dependent on the underlying cause. Consequently, BBB’s are not clinical diagnoses but rather objective signs of underlying disease. The treatment for these findings is therefore directed at the underlying disease, and may benefit from specialist consultation for assessment and management.
